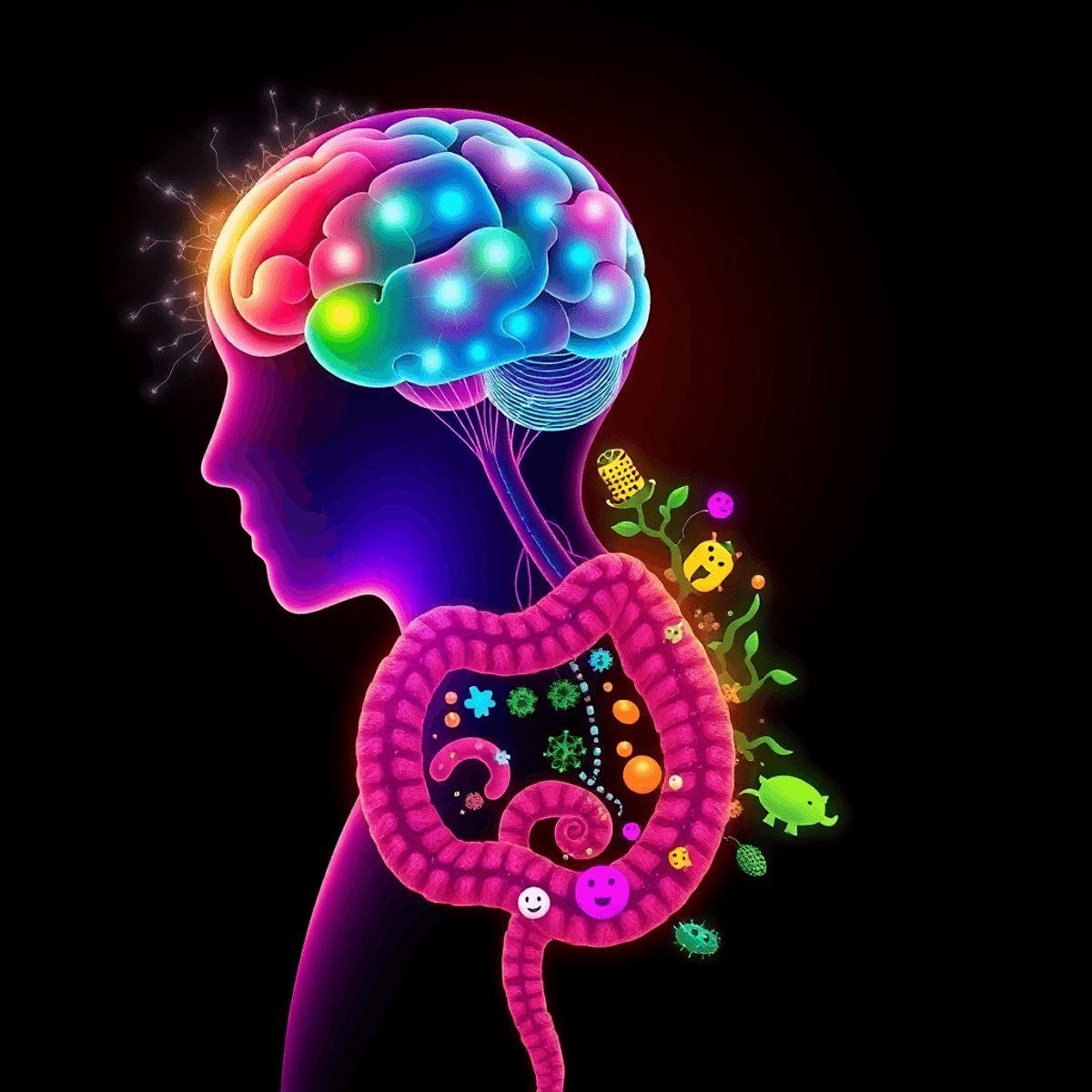
The connection between your gut health and mental well-being has become an exciting area of scientific research. Recent studies show that the bacteria in your digestive system play a crucial role in shaping your emotions, influencing everything from daily mood swings to serious mental health conditions.
Your gut contains a diverse community of microorganisms known as the gut microbiota. These tiny organisms communicate directly with your brain through a complex network called the brain-gut-microbiota axis. This biological pathway carries signals that impact:
- How you process emotions
- Your body’s response to stress
- Levels of anxiety
- Symptoms of depression
Scientists have found that changes in the composition of gut bacteria can lead to significant shifts in mood and behavior. These microscopic organisms produce neurotransmitters, which are chemical messengers that regulate emotions in the brain. When there’s an imbalance in your gut microbiota, it can disrupt this delicate communication system.
The influence of gut health on mental well-being goes beyond temporary mood swings. Research indicates that individuals with mood disorders often exhibit distinct patterns in their gut bacterial populations. This insight has opened up new possibilities for treating mental health conditions by focusing on improving gut health, representing a significant shift in psychiatric medicine.
However, maintaining a healthy gut is not just about the microorganisms living there. Other factors like proper hydration and diet also play important roles. For example, including healthy snacks for diabetes can greatly enhance overall health and well-being.
Additionally, certain treatments such as NAD+ injections have shown promise in improving cognitive function and recovery, which could indirectly benefit mental health.
Interestingly, some unconventional remedies like butterfly milk are gaining attention for their potential health benefits, including those related to gut health.
Lastly, it’s important to acknowledge that our understanding of gut health is still evolving. Recent studies have uncovered the role of gut microbes in causing constipation, highlighting the need for further research into this intricate field.
Understanding the Brain-Gut-Microbiota Axis
The brain-gut-microbiota axis is a complex communication system that connects your brain, digestive system, and the trillions of microorganisms living in your gut. This system works through:
- Neural Pathways: The vagus nerve acts as a direct link between your brain and gut
- Immune Signals: Gut bacteria influence immune cell behavior and inflammation responses
- Hormonal Messages: Chemical signals that affect mood, appetite, and stress responses
Role of Gut Microbiota
Your gut microbiota plays an active role in regulating important bodily functions. These tiny organisms produce substances that impact both the immune system and hormonal systems:
- Regulation of inflammation responses
- Production of immune-modulating substances
- Secretion of hormones affecting metabolism
- Creation of neurotransmitter precursors
Bidirectional Communication
The two-way nature of this communication system means that your mental state can affect gut function, and your gut health can influence your mental well-being. This interaction occurs through:
- Brain to Gut: Stress signals impacting digestive processes and microbiota composition
- Gut to Brain: Bacterial metabolites influencing neurotransmitter production and brain function
Research indicates that disruptions in this communication system can contribute to various mental health conditions, emphasizing the importance of maintaining a balanced gut ecosystem for psychological well-being.
Recent Findings on Weight Loss Medications
Interestingly, recent studies have shown that certain weight loss medications like Wegovy can also affect the gut microbiota. This medication not only helps with weight loss but also has implications on how we metabolize substances like alcohol.
Moreover, for individuals dealing with diabetes, Sublingual Semaglutide has emerged as a non-invasive treatment option that improves patient compliance and supports effective weight loss.
Gut Health Issues and Mental Well-being
It’s important to note that certain gut health problems such as constipation may be linked to an imbalance in gut microbes. For example, individuals experiencing [Intestinal Methanogen Overgrowth (IMO)](https://wellnesshq.net/health-news-research/symptom-profile-of-patients-with-intestinal-methanogen-overgrowth-a-systematic-review-and-meta-analysis-2) might find their condition worsened by stress or other mental health issues due to the interconnectedness of the brain-gut-microbiota axis.
Gut Microbiota and Mood Disorders
Research reveals a striking connection between altered gut microbial diversity and major mood disorders. Studies show that patients with Major Depressive Disorder (MDD) and Bipolar Disorder (BD) display distinct changes in their gut microbiome composition.
Key findings in gut microbiota alterations include:
- Reduced levels of Faecalibacterium and Coprococcus bacteria in MDD patients
- Decreased abundance of Lactobacillus and Bifidobacterium in BD individuals
- Lower diversity of beneficial microorganisms that produce butyrate
These beneficial bacteria play essential roles in:
- Producing short-chain fatty acids
- Supporting immune system function
- Maintaining intestinal barrier integrity
The presence of pro-inflammatory bacteria significantly impacts mental health conditions. Studies demonstrate increased levels of inflammatory markers in patients with mood disorders, particularly:
- Higher concentrations of Enterobacteriaceae
- Elevated levels of Bacteroides
- Increased presence of pathogenic strains
These bacterial imbalances create a pro-inflammatory environment that affects brain function through:
- Disruption of neurotransmitter production
- Alteration of immune responses
- Compromise of the intestinal barrier
Recent clinical studies highlight that patients with severe depression show up to 35% reduction in beneficial bacterial species compared to healthy individuals. This reduction correlates with symptom severity and treatment resistance in mood disorders.
Interestingly, positive experiences during childhood have been linked to better heart health, which is an important aspect of overall well-being. Moreover, adopting certain lifestyle changes such as intermittent fasting can also have beneficial effects on metabolic health, potentially influencing both physical and mental health outcomes.
Neurotransmitters, Mood Regulation, and Gut Health
Your gut microbiota acts as a natural pharmaceutical factory, producing essential neurotransmitters that directly influence your brain function and emotional well-being. Research indicates that gut bacteria synthesize and release numerous neurochemicals, including:
- Serotonin: 90% of this “feel-good” neurotransmitter originates in your gut
- GABA: The primary inhibitory neurotransmitter that reduces anxiety and promotes relaxation
- Dopamine: A key player in motivation, pleasure, and reward systems
The gut microbiota’s influence on neurotransmitter production creates a direct chemical pathway between your digestive system and brain function. Specific bacterial strains demonstrate unique capabilities in neurotransmitter synthesis:
- Lactobacillus and Bifidobacterium species produce GABA
- Escherichia and Enterococcus generate serotonin
- Bacillus species create dopamine
Disruptions in neurotransmitter metabolism can trigger significant mood alterations. When gut bacteria populations become imbalanced, neurotransmitter production may be affected in these ways:
- Reduced synthesis of mood-stabilizing compounds
- Altered neurotransmitter receptor sensitivity
- Disrupted neural signaling patterns
Research shows that patients with mood disorders often display abnormal levels of these gut-derived neurotransmitters, suggesting a strong connection between bacterial neurotransmitter production and mental health stability.
Dysbiosis, Stress Response, and Psychiatric Conditions
Dysbiosis disrupts the delicate balance of gut microorganisms, creating a ripple effect that extends beyond digestive health. Research shows a direct link between gut microbiota imbalance and various psychiatric conditions:
- Depression: Patients exhibit reduced microbial diversity
- Anxiety disorders: Associated with increased harmful bacteria
- Schizophrenia: Marked by distinct alterations in gut microbiome composition
- Autism spectrum disorders: Characterized by specific microbial patterns
The Impact of Stress on Gut Health
Stress triggers a cascade of biological responses that affect gut health through the hypothalamic-pituitary-adrenal (HPA) axis. When you experience stress, your body releases cortisol, leading to:
- Increased intestinal permeability (“leaky gut”)
- Enhanced inflammatory responses
- Altered gut microbiota composition
- Reduced beneficial bacteria populations
The stress-induced changes in gut microbiota create a self-perpetuating cycle. Your compromised intestinal barrier allows inflammatory molecules to enter the bloodstream, intensifying mood symptoms through the gut-brain axis. This biological interplay explains why stress management proves crucial for both mental health and digestive wellness.
The Connection Between Chronic Stress and Gut Microbiota
Recent studies identify specific bacterial strains affected by chronic stress, including reduced Lactobacillus and Bifidobacterium populations. These changes correlate with increased severity of psychiatric symptoms, highlighting the intricate relationship between stress response, gut health, and mental well-being.
The Role of Weight Management in Overall Wellness
Interestingly, managing weight can also play a role in overall wellness. For instance, medications like Phentermine and Ozempic, each with their unique benefits and side effects, are often used for effective weight management.
In some cases, individuals on Ozempic might experience prolonged fullness after meals due to its effects on satiety. Understanding this phenomenon can help manage dietary habits while on the medication – here’s a detailed guide on that.
Additionally, for those managing Type 2 diabetes, comparing Jardiance and Ozempic could provide valuable insights into their respective benefits for diabetes care.
The Mind-Body Connection
Lastly, it’s essential to remember that our mental health is closely tied to our physical well-being. Hence, incorporating strategies for better sleep and relaxation could further aid in managing stress levels and improving overall health. Additionally, recent research suggests that understanding the complex relationship between dysbiosis and mental health could lead to more effective treatment strategies for psychiatric conditions (source).
Interventions for Mood Disorders: Targeting Gut Health
Research reveals promising therapeutic approaches targeting gut health to address mood disorders. Probiotics emerge as powerful tools in mental health treatment, with specific strains showing remarkable effects:
- Lactobacillus and Bifidobacterium species reduce anxiety-like behaviors
- Lactobacillus rhamnosus increases GABA receptor expression
- Multi-strain probiotic supplements improve depression scores
Fecal Microbiota Transplantation (FMT) demonstrates significant potential in treating mood disorders through microbiome restoration. Animal studies highlight FMT’s effectiveness:
- Mice receiving FMT from depressed humans develop depression-like behaviors
- FMT from healthy donors reverses anxiety and depression symptoms
- Behavioral improvements correlate with restored microbial diversity
Recent clinical trials support these findings:
“FMT recipients reported 50% reduction in depression symptoms after 8 weeks, with sustained improvements at 6-month follow-up” – Journal of Psychiatric Research
The gut-targeting interventions show particular promise in treatment-resistant cases. Patients unresponsive to traditional antidepressants experience symptom improvement when combining conventional treatments with microbiome-focused therapies.
These approaches represent a shift toward integrated treatment strategies that acknowledge the gut-brain connection in mental health care. Furthermore, exploring menopause-friendly nutrition can also play a significant role in overall wellness during this transition, particularly for women experiencing mood disorders related to menopause.
Additionally, adopting practices like the 96-hour fast can enhance gut health and potentially improve mental health outcomes.
Gastrointestinal Disorders, Emotional Well-being, and Therapeutic Approaches
Research reveals a strong connection between Irritable Bowel Syndrome (IBS) and mental health conditions. Up to 60% of IBS patients experience concurrent depression or anxiety disorders, creating a complex interplay between digestive symptoms and emotional distress.
The bidirectional relationship between IBS and mood disorders manifests through:
- Physical Symptoms: Abdominal pain, bloating, and altered bowel habits intensify during periods of emotional distress
- Psychological Impact: Chronic digestive issues lead to increased anxiety and depressive symptoms
- Social Consequences: Both conditions can limit daily activities and social interactions
Therapeutic approaches targeting both gut health and emotional well-being show promising results. Integrated treatment strategies include:
Combined Medication Protocols
- Antidepressants at low doses help manage both IBS symptoms and mood
- Gut-specific medications paired with anxiety-reducing agents
Mind-Body Interventions
- Cognitive Behavioral Therapy reduces IBS severity and improves mood
- Gut-directed hypnotherapy alleviates digestive symptoms
- Mindfulness practices decrease stress-related gut inflammation
Recent clinical studies demonstrate that patients receiving combined treatments experience a 40-50% reduction in both GI symptoms and psychological distress. These findings highlight the importance of addressing both physical and emotional aspects when treating gastrointestinal disorders.
However, some medications like Ozempic, which is often used for managing Type 2 diabetes, have been reported to cause gastrointestinal side effects including bowel injuries. It’s crucial to consider such risks when opting for medication as part of the treatment strategy. Moreover, if you are pregnant or planning to become so, it’s essential to understand that Ozempic is not considered safe during pregnancy, making it necessary to explore alternative treatments.
On the emotional well-being front, holistic stress management techniques such as mindfulness, physical activity, and breath control can significantly contribute to achieving a balanced state of well-being.
Conclusion
Research reveals the profound impact of gut microbiota on mental health through multiple pathways. The intricate relationship between gut health and mood disorders operates through:
- Immune system modulation
- Neurotransmitter production
- Endocrine signaling
- Vagus nerve communication
These findings open new possibilities for mental health treatment. Emerging diagnostic markers include:
- Gut microbiome composition analysis
- Inflammatory biomarker testing
- Intestinal permeability assessment
Promising therapeutic strategies targeting gut health show potential in improving mental health outcomes:
- Personalized probiotic interventions
- Dietary modifications – Master the art of a balanced diet with essential tips on nutrition, food groups, and incorporating healthy choices for optimal health.
- Microbiota-based treatments
- Integrated mind-body approaches
The growing understanding of the brain-gut-microbiota axis transforms our approach to mood disorders. This knowledge creates opportunities for innovative treatments that address both gut health and mental well-being, marking a significant shift in psychiatric care. Future research will likely uncover additional connections, leading to more effective, targeted interventions for individuals struggling with mood disorders.
Additionally, it’s important to remember that regular exercise has numerous benefits for mental health, which can be an integral part of a holistic approach towards managing mood disorders.
FAQs (Frequently Asked Questions)
What is the brain-gut-microbiota axis and why is it important in mental health?
The brain-gut-microbiota axis is a bidirectional communication system linking the gut microbiota with neuroimmune and neuroendocrine functions of the brain. Understanding this axis is crucial as it significantly impacts mood regulation and mental health outcomes.
How does gut microbiota diversity relate to mood disorders like depression and bipolar disorder?
Altered gut microbial diversity, including decreased levels of beneficial bacteria and increased pro-inflammatory bacteria, has been linked to major depressive disorder (MDD) and bipolar disorder (BD). These changes can influence mood regulation and contribute to the pathophysiology of these disorders.
In what ways do neurotransmitters like GABA, serotonin, and dopamine connect gut health to mood regulation?
Gut microbiota affect the secretion and metabolism of key neurotransmitters such as GABA, serotonin, and dopamine. Imbalances in these neurotransmitters due to altered gut microbiota can disrupt mood regulation and are associated with mood disorders.
What role does dysbiosis play in psychiatric conditions and stress response?
Dysbiosis, or imbalance in gut microbiota, is associated with functional bowel disorders and psychiatric conditions including depression, anxiety, and schizophrenia. Stress influences gut microbiota composition through HPA axis activation, increasing cortisol secretion that affects intestinal permeability and inflammation, thereby exacerbating mood symptoms via the gut-brain axis.
Can interventions targeting gut health improve symptoms of mood disorders?
Yes, interventions such as probiotics and fecal microbiota transplantation (FMT) have shown potential benefits in alleviating symptoms of mood disorders. Evidence from animal models supports targeting gut health as a promising therapeutic strategy for mental health improvement.
How are gastrointestinal disorders like IBS connected to emotional well-being and what therapies are effective?
Irritable bowel syndrome (IBS) often co-occurs with depression and anxiety disorders. Combining antidepressants with mind-body therapies has proven effective in managing gastrointestinal symptoms while enhancing emotional well-being, highlighting the importance of integrated therapeutic approaches.