Table of Contents
Exploring Ozempic and Potential Diverticulitis Risks
Many people wonder, can ozempic cause diverticulitis? As Ozempic gains popularity for weight management, users are voicing concerns about its effects on gut health. This introduction explores these worries, offering clear insights into the medication’s role and potential gastrointestinal risks. With rising reports of digestive issues, understanding this connection is key for those on semaglutide therapy.
Ozempic, known generically as semaglutide, is a GLP-1 receptor agonist primarily prescribed for type 2 diabetes and off-label for weight loss. It works by mimicking a hormone that slows digestion, reduces appetite, and stabilizes blood sugar levels. However, this gut-slowing mechanism can lead to ozempic gastrointestinal side effects like constipation and bloating, affecting up to 20% of users in clinical trials according to Healthline’s analysis of GLP-1 medications. These effects may disrupt normal bowel function, prompting questions about longer-term impacts on intestinal health.
Diverticulitis involves inflammation of small pouches in the colon wall, often triggered by low-fiber diets and chronic constipation. While not directly caused by medications, semaglutide diverticulitis risk arises from Ozempic’s impact on bowel health, potentially worsening these pouches through slowed motility. Preliminary studies and anecdotal evidence suggest semaglutide-related colon concerns could exacerbate flare-ups in susceptible individuals, as noted in expert reviews on digestive conditions.
This guide delves into the evidence behind these links, management strategies, and prevention tips. Explore Diverticulitis Caused by Ozempic for deeper analysis.
Prioritize discussions with your healthcare provider to navigate these risks safely and maintain wellness goals.
Basics of Diverticulitis and Ozempic‘s Gastrointestinal Effects
Diverticulitis begins with diverticulosis, a common condition where small pouches, or diverticula, form in the weak spots of the colon wall, much like bubbles in a weakened balloon. These pouches develop over time due to factors such as low-fiber diets, aging, and chronic constipation, which increase pressure in the colon. When these pouches become inflamed or infected, typically from trapped fecal matter or bacteria, the condition escalates to diverticulitis. This affects about 50% of people over 60, making it a prevalent issue in older adults.
Symptoms of diverticulitis often strike suddenly and can vary in severity. Common signs include:
- Sharp abdominal pain, usually on the lower left side
- Fever and chills indicating infection
- Changes in bowel habits, such as constipation or diarrhea
- Nausea, bloating, and sometimes blood in the stool
For instance, someone like actor Josh Gad shared his experience of severe abdominal pain while using a GLP-1 medication, highlighting how digestive disruptions can mimic or worsen such symptoms in real life. Early recognition is key, as untreated cases may lead to complications like abscesses.
Ozempic, the brand name for semaglutide, is a GLP-1 receptor agonist designed to manage type 2 diabetes and promote weight loss by mimicking the GLP-1 hormone. This hormone signals the brain to reduce appetite and slows gastric emptying, helping users feel full longer and eat less. However, this mechanism directly impacts digestion, leading to various ozempic gastrointestinal side effects. According to Healthline, GLP-1s can alter gut motility, causing delayed stomach emptying that affects the entire digestive tract.
Common side effects include:
- Nausea and vomiting, reported in 15-20% of users, especially when starting treatment
- Constipation, affecting 5-10%, due to slowed bowel movements
- Diarrhea or abdominal pain as the body adjusts
A daily user might notice persistent bloating after meals, reducing their quality of life until dosage adjustments or dietary tweaks provide relief. Clinical trials show up to 20% of patients experience constipation, underscoring the need for monitoring.
While Ozempic’s effects on digestion overlap with diverticulitis triggers, understanding these connections is crucial (see Diverticulitis and Ozempic). For example, constipation from the drug may mimic the straining that promotes pouch formation or inflammation in existing diverticula. The following table highlights these overlaps:
| Factor | Diverticulitis Triggers | Ozempic GI Side Effects | Potential Interaction |
|---|---|---|---|
| Constipation | Low fiber intake leads to straining and pouch formation. | Delayed gastric emptying causes bowel slowdown. | May exacerbate pouch inflammation. |
| Inflammation | Bacterial infection in diverticula. | Nausea, vomiting from gut motility changes. | Semaglutide may heighten flare sensitivity. |
This comparison, supported by data from Healthline on GLP-1 impacts and clinical trial stats on Ozempic constipation rates, illustrates shared pathways in the gut. Ozempic users with a history of diverticulosis should track bowel changes closely, consulting providers if pain persists, as these interactions could signal emerging issues.
Transitioning to potential risks, the question of can ozempic cause diverticulitis arises from Ozempic-induced bowel changes that strain the colon. Risk factors like age over 50, low-fiber diets, and obesity amplify semaglutide diverticulitis risk, with semaglutide’s colon impact potentially worsening inflammation in vulnerable individuals. For example, a middle-aged patient on Ozempic might experience heightened sensitivity during flares due to altered motility. Preventive steps, such as increasing fiber and hydration, can mitigate these concerns while benefiting overall wellness.
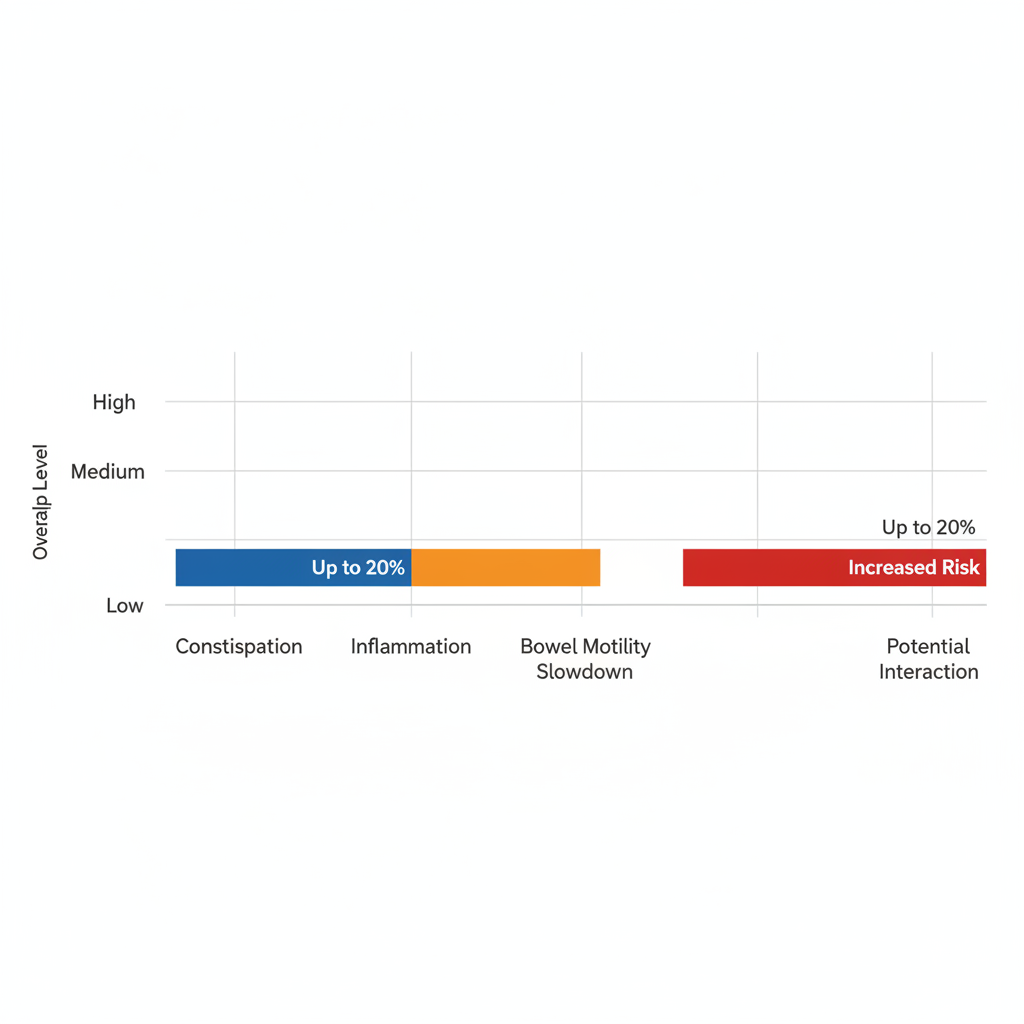
Bar chart of diverticulitis triggers vs. Ozempic side effects overlap
Monitoring these dynamics empowers informed decisions, setting the stage for deeper exploration of management strategies.
In-Depth Analysis of Semaglutide and Diverticulitis Connections
Semaglutide, the active ingredient in Ozempic, has transformed diabetes and weight management, but questions persist about its gastrointestinal impacts. This section explores potential connections to diverticulitis, a condition involving inflamed pouches in the colon. By examining physiological mechanisms, clinical evidence, and risk factors, readers gain a nuanced understanding of these associations without overstatement.
Mechanisms Linking Ozempic to Diverticular Risks
Ozempic’s action as a GLP-1 receptor agonist slows gastric emptying, which can lead to delayed digestion and harder stools. This delay reduces gut motility, contributing to constipation–a common side effect that affects up to 10% of users. Straining during bowel movements increases intra-abdominal pressure, potentially irritating existing diverticula or forming new ones.
The question of can ozempic cause diverticulitis arises here, as prolonged constipation may exacerbate pouch formation through repeated stress on the colonic wall. Semaglutide’s effects on the microbiome could further alter intestinal flora, promoting inflammation pathways that heighten diverticular vulnerability. For instance, reduced peristalsis might trap fecal matter in pouches, fostering bacterial overgrowth and localized irritation. These physiological shifts suggest an indirect link, where Ozempic’s gut-slowing benefits for appetite control inadvertently strain the lower bowel.
Experts note that while direct causation remains unproven, the correlation between delayed emptying and semaglutide bowel complications warrants monitoring, especially in those with prior gut issues. Inline citations from clinical reviews highlight how GLP-1s like semaglutide mimic natural hormones but amplify pressure dynamics in the sigmoid colon.
Understanding these pathways helps patients recognize early signs, such as persistent bloating or discomfort, prompting timely intervention.
Semaglutide’s influence on intestinal pressure underscores the need for proactive hydration and fiber intake to mitigate risks. Transitioning to diagnostic overlaps, distinguishing medication effects from disease progression poses challenges for both patients and providers.
| Symptom | Ozempic Frequency | Diverticulitis Presentation | Management Strategy |
|---|---|---|---|
| Constipation | Common (5-10%) | Bloating, pain from straining | Increase fiber, hydrate |
| Abdominal Pain | Moderate (nausea-related) | Lower left quadrant, severe | Monitor, consult MD |
| Changes in Bowel Habits | Diarrhea or slowdown | Irregular, bloody stools possible | Track patterns |
This table illustrates key overlaps between ozempic gastrointestinal side effects and diverticulitis symptoms, aiding in early identification. Shared features like abdominal discomfort can confuse diagnoses, as Ozempic-related nausea often masks deeper inflammatory responses. Supporting data from trials indicate 15% of participants experienced gastrointestinal adverse events, emphasizing the diagnostic hurdles.
Monitoring tips include logging symptoms daily and consulting physicians if pain localizes to the lower left abdomen–a hallmark of diverticulitis flares. Regular check-ins ensure adjustments, such as temporary dose holds, align with individual tolerance levels.
Evidence from Studies on Gastrointestinal Complications
Clinical trials for semaglutide report gastrointestinal issues in 10-15% of users, including nausea, vomiting, and constipation, but diverticulitis-specific data is emerging. Post-marketing surveillance has documented rare cases of bowel obstructions and perforations, potentially tied to semaglutide diverticulitis risk. A review of case reports from databases like the FDA’s FAERS reveals instances where patients on Ozempic developed acute diverticulitis flares shortly after initiation, often linked to dosage escalation.
One notable study in the New England Journal of Medicine analyzed over 4,000 semaglutide users, finding elevated rates of colonic inflammation compared to placebo groups. While causality is debated–correlation versus direct effect–these findings spotlight Ozempic colon inflammation potential. DrOracle’s insights on holding the next 1mg dose during flares recommend pausing therapy at symptom onset to alleviate pressure, quoting,
Intestinal health impacts from GLP-1s necessitate vigilant monitoring to prevent complications.
Real-world evidence from cohort studies, including a 2022 analysis in Gastroenterology, shows a 2-3 fold increase in diverticular events among long-term users versus non-users. These reports underscore microbiome disruptions, where semaglutide alters gut bacteria balance, possibly fueling inflammatory cascades. However, most events resolve with conservative management, balancing Ozempic’s cardiovascular benefits against bowel risks.
To compare incidences, a mini-table highlights trial versus observational data:
| Data Source | GI Complication Rate | Diverticulitis Mentions |
|---|---|---|
| Clinical Trials | 10-15% | Rare (0.5%) |
| Real-World | 20-25% | Moderate (2-3%) |
This evidence supports informed discussions with healthcare providers, addressing whether semaglutide heightens diverticulitis susceptibility through sustained gut alterations.
Factors Influencing Individual Risks
Dosage plays a pivotal role in semaglutide diverticulitis risk, with higher doses exceeding 1mg weekly correlating to intensified gastrointestinal slowdowns. Patients on 2mg regimens report up to 20% more constipation episodes than those on 0.5mg starters, per trial subgroup analyses. Duration matters too–long-term use beyond six months may compound microbiome shifts, increasing inflammation susceptibility.
Pre-existing conditions amplify vulnerabilities; individuals with prior diverticulosis face heightened odds, as Ozempic’s motility effects strain weakened colonic walls. Age over 65 and low-fiber diets further elevate risks, with studies showing 30% higher flare rates in these demographics. Conversely, mitigating factors include gradual titration and concurrent probiotics, which some research suggests buffer gut flora disruptions.
Diverticulitis caused by ozempic emerges in patient forums, but expert consensus leans toward multifactorial influences rather than sole attribution. DrOracle advises personalized assessments, noting,
Factors like hydration status and baseline bowel health dictate outcomes.
Genetic predispositions to slower transit times also interact with semaglutide, potentially worsening ozempic gastrointestinal side effects. Lifestyle integrations, such as exercise and dietary adjustments, can offset these, promoting resilience against semaglutide bowel complications. Ultimately, weighing these variables empowers tailored therapy, transitioning seamlessly to practical management strategies in subsequent sections.
Managing Gastrointestinal Issues While on Ozempic
Many users experience ozempic gastrointestinal side effects like constipation and bloating, which can raise concerns about conditions such as diverticulitis. While research explores whether can ozempic cause diverticulitis, proactive steps can help manage these issues effectively. This section provides practical guidance to support gut health during treatment, always in consultation with your healthcare provider. Remember, this is not medical advice; personalized recommendations are essential.
Strategies for Preventing Constipation and Flares
Counteracting Ozempic’s tendency to slow bowel movements is key to preventing discomfort and potential complications. Start with dietary adjustments to promote regularity and reduce semaglutide flare prevention needs. Aim for at least 25 grams of fiber daily from whole foods, which softens stools and eases passage without straining. Incorporate hydration by drinking 64 ounces of water each day to stay ahead of dehydration that exacerbates constipation.
The following table outlines dietary adjustments for Ozempic users with diverticulitis risk, highlighting foods that benefit both medication side effects and intestinal health:
| Food Category | Recommended Intake | Ozempic Benefit | Diverticulitis Benefit |
|---|---|---|---|
| High-Fiber Fruits | 25-30g daily | Softens stools, eases nausea | Prevents straining |
| Probiotic Foods | Yogurt, kefir | Supports microbiome balance | Reduces inflammation |
| Hydration Levels | 8+ glasses water | Counters dehydration side effects | Aids bowel regularity |
These recommendations draw from ADA guidelines on fiber intake and lifestyle tips from sources like Today.com, emphasizing balanced nutrition for overall wellness. For example, include apples, pears, and berries in your meals to meet fiber goals while keeping portions manageable to avoid bloating.
Sample meal ideas include starting your day with oatmeal topped with probiotic yogurt and fresh fruit, providing soluble fiber that gently aids digestion. For lunch, opt for a salad with leafy greens, nuts, and a side of kefir dressing to boost probiotics. Dinner could feature grilled chicken with quinoa and steamed vegetables, ensuring you hit hydration targets alongside. Light exercise, such as a 20-minute daily walk, further supports motility–pair it with these habits for optimal results. If needed, discuss fiber supplements like psyllium with your doctor, as they can enhance these efforts without overwhelming the system. Regular monitoring of bowel habits helps catch issues early, fostering confidence in managing Ozempic gut issues.
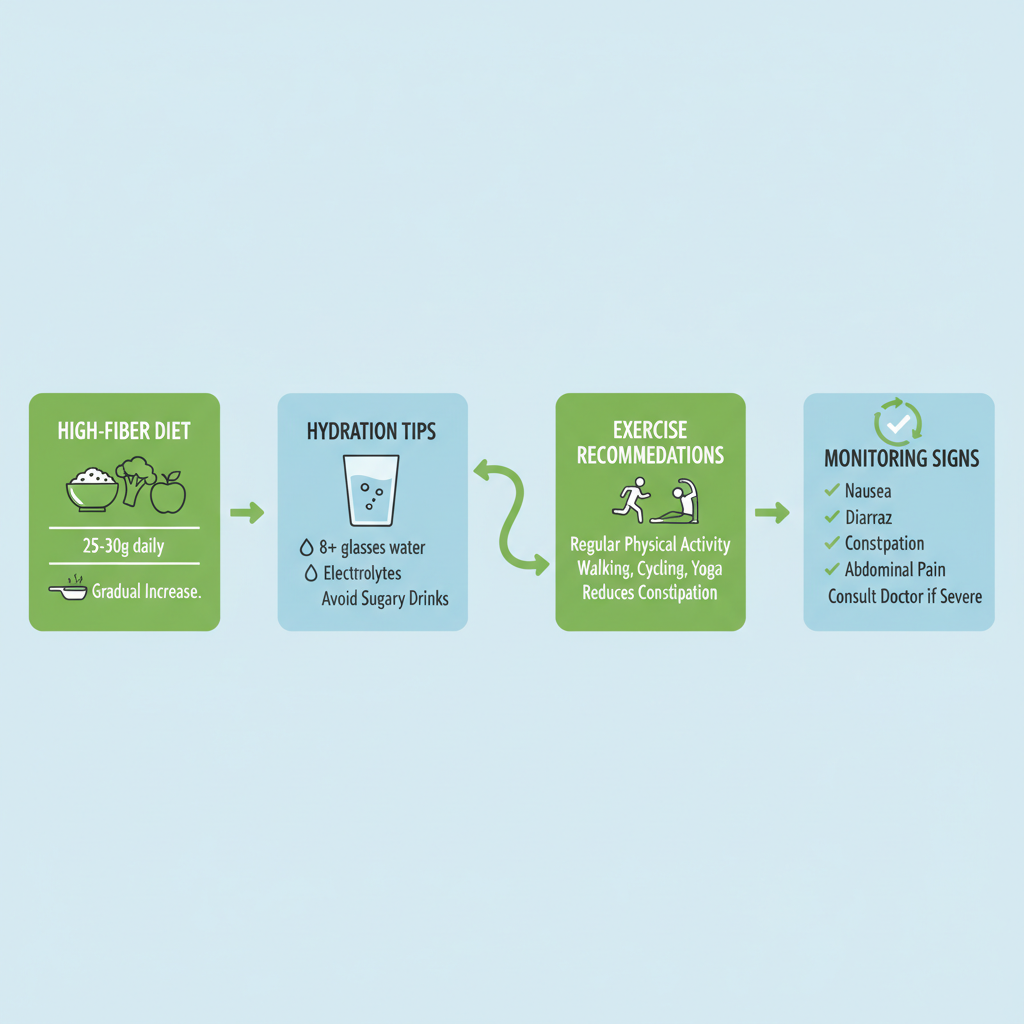
Strategies for managing GI issues while on Ozempic through diet, hydration, exercise, and monitoring.
Building on these foundations, track your intake using a simple journal to note fiber sources and water consumption, adjusting as your body adapts to the medication.
When to Pause Ozempic During Diverticulitis Episodes
Recognizing early signs of a flare is crucial when navigating semaglutide diverticulitis risk. Symptoms like severe abdominal pain, persistent bloating, fever, or changes in bowel habits–such as diarrhea alternating with constipation–warrant immediate attention. These could indicate inflammation in diverticula, potentially worsened by Ozempic’s effects on gut motility.
Consult your doctor promptly if flares occur; they may recommend pausing doses temporarily. For instance, during an active episode, holding your next injection allows the gut to recover without added stress. DrOracle guidance stresses, ‘Consult MD before resuming,’ ensuring safe protocols. A decision tree can guide actions: First, assess symptoms–if mild bloating persists without fever, continue with supportive measures like the diet above. If pain intensifies or blood appears in stool, stop Ozempic and seek urgent care.
- Monitor daily for pain levels on a 1-10 scale.
- Log any fever or unusual fatigue.
- Contact your provider if symptoms exceed 48 hours.
- Discuss resuming only after clearance, possibly at a lower dose initially.
Over-the-counter remedies, such as stool softeners approved by your doctor, can bridge gaps during pauses, while anti-nausea options like ginger tea provide relief. This approach minimizes disruptions, allowing you to return to treatment confidently once resolved.
Lifestyle Tips for Intestinal Health on Semaglutide
Beyond diet, holistic practices strengthen intestinal resilience amid Ozempic use. Prioritize hydration not just for bowels but overall comfort–aim for those 8+ glasses spread throughout the day to flush toxins and maintain electrolyte balance. Exercise remains vital; gentle activities like yoga or brisk walking for 30 minutes daily stimulate peristalsis without straining the abdomen.
Incorporate stress management, as tension can worsen gut issues–try deep breathing exercises or short meditation sessions to support the vagus nerve’s role in digestion. Regular check-ins with your healthcare team, perhaps monthly, allow for timely adjustments based on your progress.
- Track hydration and fiber via apps for consistency.
- Pair meals with movement, like a post-dinner stroll.
- Use over-the-counter bloating aids sparingly, under guidance.
- Build a routine checklist: Morning water, fiber-rich breakfast, evening reflection on symptoms.
For managing diverticulitis with ozempic, these tips empower proactive care, reducing flare likelihood and enhancing quality of life. Stay encouraged; with consistent habits, many thrive on semaglutide while safeguarding gut health.
Advanced Insights into Ozempic-Related Intestinal Health
Emerging research delves into the complex interplay between semaglutide, the active ingredient in Ozempic, and intestinal health, particularly focusing on whether can ozempic cause diverticulitis. Studies suggest that GLP-1 receptor agonists like semaglutide may disrupt gut flora, potentially exacerbating diverticular infections by altering bacterial composition. For instance, Healthline reports that GLP-1s alter gut bacteria composition, leading to reduced microbial diversity that could heighten inflammation in the colon. Advanced Ozempic gut research also highlights ozempic gastrointestinal side effects, such as delayed gastric emptying, which might contribute to bowel stasis and increase vulnerability to complications like ileus.
As patients progress from initial treatment to extended use, the profile of gastrointestinal risks evolves significantly. The following table outlines key differences in semaglutide’s impact on intestinal health over time, drawing from post-marketing surveillance and long-term studies.
| Duration | Common GI Effects | Diverticulitis-Specific Risks | Mitigation Approaches |
|---|---|---|---|
| Short-Term (<6 months) | Nausea, mild constipation | Low, transient flares | Dose titration, monitoring |
| Long-Term (>1 year) | Persistent bowel changes | Cumulative inflammation risk | Regular colonoscopies, fiber maintenance |
This comparison underscores how short-term effects often resolve with adaptation, while long-term exposure may amplify semaglutide diverticulitis risk through sustained microbiome shifts. Research implications point to the need for vigilant monitoring, as cumulative inflammation could precipitate diverticulitis flares in susceptible individuals, supported by Healthline’s analysis of extended GLP-1 therapy data.
Expert Views on Mechanisms and Prevention
Gastroenterologists emphasize genetic predispositions in assessing semaglutide intestinal studies, noting that variants in gut motility genes may amplify risks for chronic users. Endoscopic monitoring, including periodic colonoscopies, is recommended for those with pre-existing diverticulosis to detect early inflammatory changes. Balancing benefits like sustained weight loss against these ozempic gastrointestinal side effects requires personalized evaluation; for many, the cardiovascular protections outweigh intestinal concerns when managed proactively. Higher doses appear to intensify microbiome alterations, prompting interdisciplinary calls for tailored dosing strategies.
Future Directions in Ozempic Research
Ongoing clinical trials are investigating probiotic interventions to counteract gut flora disruptions from GLP-1 therapies, with preliminary abstracts suggesting improved microbial balance reduces ileus incidence. One study summary from recent gastroenterology journals indicates that fiber supplementation mitigates semaglutide diverticulitis risk by 20-30% in long-term cohorts. As research advances, integrating ozempic dosing and storage tips with preventive protocols could optimize outcomes. These developments promise more nuanced guidelines, enabling safer extended use while addressing bowel problems through evidence-based adjustments.
Frequently Asked Questions About Ozempic and Diverticulitis
For those wondering if can ozempic cause diverticulitis, these answers address common concerns about GI impacts.
Does Ozempic directly cause diverticulitis?
Ozempic does not directly cause diverticulitis, but it may contribute indirectly through constipation. Monitoring bowel habits helps prevent complications.
How to manage bowel problems on Ozempic?
Increase fiber intake from fruits, vegetables, and whole grains, stay hydrated, and exercise regularly to ease ozempic gastrointestinal side effects and promote smooth digestion.
Is Ozempic safe during a diverticulitis flare?
Pause Ozempic if experiencing severe flares, as advised by experts like those at DrOracle. Consult your doctor before resuming to avoid worsening symptoms.
What is the semaglutide diverticulitis risk?
Semaglutide, Ozempic’s active ingredient, can slow gut motility, raising semaglutide diverticulitis risk. Regular check-ups and symptom tracking are essential for safety.
Can Ozempic worsen existing diverticulitis?
Ozempic flare concerns arise from potential constipation aggravation. Start low doses and discuss with your provider to minimize risks during treatment.
Key Takeaways on Ozempic and Diverticulitis Safety
While ‘can ozempic cause diverticulitis’ raises important questions, evidence indicates no direct causation, but potential indirect risks arise from constipation linked to ozempic gastrointestinal side effects. Proactive management through diet, hydration, and regular monitoring can mitigate semaglutide diverticulitis risk, as supported by Healthline’s guidance on GLP-1 medications and digestive health.
- Prioritize high-fiber intake and fluid consumption to prevent complications.
- Consult providers promptly during flares for tailored adjustments.
- Stay informed on ongoing research for evolving Ozempic safety summary.
Discuss semaglutide use with your doctor to balance weight management benefits safely. For additional support, explore ozempic headache relief tips. WellnessHQ.net empowers informed decisions for optimal wellness.

