Table of Contents
Understanding Ozempic and Diverticulitis Risks
Many people starting Ozempic for weight loss or diabetes management wonder, can ozempic cause diverticulitis flare up? This question highlights growing concerns about the Does Ozempic Cause Diverticulitis potential, especially for those with gastrointestinal histories. Ozempic, known generically as semaglutide, is a GLP-1 receptor agonist that mimics hormones to regulate blood sugar levels and reduce appetite. By slowing gastric emptying, it helps control hunger but can influence digestive processes in ways that raise questions about the ozempic diverticulitis connection.
Diverticulitis occurs when small pouches, or diverticula, in the colon become inflamed or infected, often due to trapped waste. It’s common, affecting about 50% of people over 60 with diverticulosis, the precursor condition. Risk factors include advancing age, low-fiber diets, and sedentary lifestyles, which can weaken colon walls and promote bacterial buildup. For those on Ozempic, understanding semaglutide and colon inflammation risks becomes crucial, as the drug’s effects on bowel motility might indirectly contribute to flare-ups.
Common ozempic constipation side effects, alongside nausea and vomiting, stem from delayed digestion, potentially altering stool consistency and increasing colon pressure. While direct causation remains under study, GLP-1 agonists bowel impact could exacerbate existing vulnerabilities. Patient experiences, as shared in wellness resources, emphasize monitoring symptoms like abdominal pain or changes in bowel habits to navigate this journey safely.
This guide explores the fundamentals, mechanisms, practical tips, and management strategies ahead. To grasp if Ozempic might trigger issues, let’s delve into the basics of both the drug and condition. Always consult your healthcare provider for personalized advice tailored to your health profile.
Basics of Ozempic and Diverticulitis
Ozempic, a popular medication for type 2 diabetes and weight management, has sparked interest in its potential effects on gastrointestinal health. This section explores the fundamentals of Ozempic alongside diverticulitis, a common colon condition, to help readers understand their interplay. By breaking down how each works and possible connections, we address key concerns like the potential for Ozempic to influence gut health.
Ozempic contains semaglutide, a synthetic version of the GLP-1 hormone that regulates blood sugar and appetite. Administered as a weekly subcutaneous injection, it starts at a low dose of 0.25 mg to minimize side effects, gradually increasing to 1 mg or 2 mg based on patient response. Semaglutide mimics natural GLP-1 by stimulating insulin release, slowing gastric emptying, and promoting satiety, which aids weight loss. This mechanism, often likened to putting a brake on the digestive conveyor belt, reduces post-meal glucose spikes effectively. Compared to similar GLP-1 drugs like Wegovy, Ozempic shares the core action but is primarily approved for diabetes control, though off-label weight loss use is widespread. Clinical data shows it can lead to 5-10% body weight reduction over six months, making it a go-to for obesity management.
Diverticulitis involves small pouches, or diverticula, forming in the colon wall, a condition known as diverticulosis when asymptomatic. When these pouches become inflamed or infected, it progresses to diverticulitis, causing abdominal pain, fever, and digestive changes. Unlike diverticulosis, which affects up to 50% of people over 60 in the US, diverticulitis strikes about 4-5% of those with pouches, often triggered by bacterial overgrowth or trapped fecal matter. Risk factors include a low-fiber diet, obesity, lack of exercise, and aging, as weak colon spots bulge under pressure from hard stools. High-fiber intake and hydration help prevent flares by softening stool and easing bowel movements. Understanding this distinction is crucial, as many live with silent diverticulosis without issues.
Common GI side effects of Ozempic affect 30-40% of users, including nausea, vomiting, and ozempic constipation side effects that can persist for weeks. These arise from delayed gastric emptying in about 20% of patients, as noted in clinical studies on semaglutide bowel complications. Other effects involve diarrhea or abdominal discomfort, though most subside over time. Monitoring hydration and fiber intake is essential to manage these, and patients with pre-existing gut issues should consult providers.
Ozempic’s broad impact on the digestive system warrants a closer look at specific conditions. The following table compares its effects on diverticulitis versus other GI issues like GERD and IBS, drawing from reported mechanisms and prevalence data.
| Condition | Ozempic Mechanism | Risk of Flare-Up | Prevalence with Ozempic |
|---|---|---|---|
| Diverticulitis | Slowed gastric emptying leading to constipation | Indirect via constipation (Moderate) | 10-15% of users report GI issues |
| GERD | Nausea and delayed emptying | Direct aggravation (High) | 20% increase in symptoms |
| IBS | Bowel motility changes | Variable (Low to moderate) | 5-10% affected |
This comparison highlights how Ozempic influences gut motility across conditions, with constipation emerging as a key factor linking to diverticulitis risks. For instance, hardened stools from slowed transit can pressure colon pouches, potentially worsening inflammation. Data from clinical trials and patient reports underscore the need for proactive management, such as stool softeners, to mitigate these effects.
When exploring the ozempic diverticulitis connection, questions arise about whether it can directly trigger issues or exacerbate existing ones. Initial evidence suggests an indirect pathway through gastrointestinal slowdowns, raising concerns around can ozempic cause diverticulitis flare up in susceptible individuals. The Ozempic and Diverticulitis interaction primarily ties to GLP-1 drugs and colon health via constipation, with studies indicating moderate risk for those with diverticulosis. While not a primary side effect, awareness and regular check-ups are advised to balance benefits against potential semaglutide bowel complications.
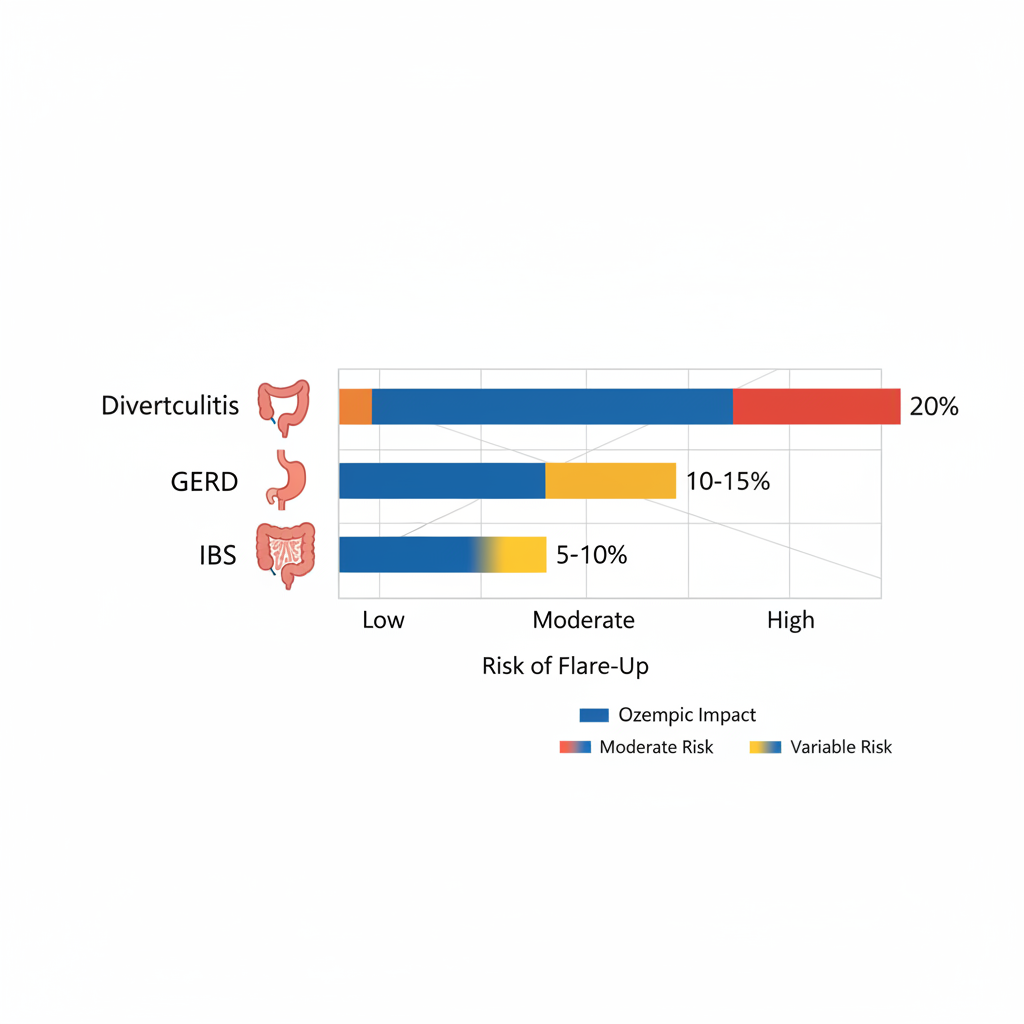
Bar chart of Ozempic’s effects on common gastrointestinal conditions like Diverticulitis, GERD, and IBS.
Discussing these basics reveals the nuanced relationship between medication and gut health. With these foundations, let’s examine the scientific evidence and mechanisms in detail.
Scientific Evidence on Ozempic and Diverticulitis
Ozempic, known generically as semaglutide, has garnered attention for its role in managing type 2 diabetes and weight loss, but concerns persist about its gastrointestinal impacts. This section examines the scientific basis for potential links between Ozempic and diverticulitis flare-ups, drawing on mechanisms, studies, and risk factors. While direct causation remains unproven, indirect pathways through gut changes warrant careful consideration.
Mechanisms of Potential Flare-Ups
The question of whether Ozempic can cause diverticulitis flare-ups centers on its influence on gastrointestinal function. Semaglutide, a GLP-1 receptor agonist, slows gastric emptying and gut motility, reducing transit time by 20-30% in many users. This delay often manifests as ozempic constipation side effects, where stool hardens and movement stalls, increasing intra-colonic pressure.
Such pressure buildup strains existing diverticula–small pouches in the colon wall–potentially leading to micro-tears and bacterial invasion. Inflammation follows, escalating into acute diverticulitis. Semaglutide-induced bowel strain exacerbates this by altering the gut microbiome, promoting dysbiosis that favors pathogenic bacteria. GLP-1 constipation complications compound the issue, as chronic constipation heightens diverticular pouch distension. Studies indicate these motility changes contribute to GI adverse events in about 40% of patients, though not all progress to severe inflammation. More research is needed to quantify exact thresholds, but the physiological chain–delayed transit to pressure to pouch rupture–offers a plausible explanation for flare-up risks.
To contextualize these class-wide effects, the table below compares constipation and diverticulitis-related outcomes across select GLP-1 agonists, highlighting semaglutide’s profile.
| Drug | Constipation Incidence | Diverticulitis Reports | Study Source |
|---|---|---|---|
| Ozempic (Semaglutide) | 25-30% | Indirect links via case reports | PMC and clinical trials |
| Wegovy (Semaglutide higher dose) | 30-35% | Similar indirect risks; higher due to dose | FDA data; post-marketing |
| Trulicity (Dulaglutide) | 20-25% | Fewer reports; low | Comparative studies; journal reviews |
Based on meta-analyses, these figures underscore semaglutide’s moderate constipation rate, which correlates with potential bowel strain. Ozempic shows more frequent reports of indirect GI complications compared to dulaglutide, possibly due to dosing differences. This comparison aids in understanding relative risks within the GLP-1 family, emphasizing the need for monitoring in susceptible individuals. Implications suggest that while Ozempic’s benefits outweigh risks for many, proactive management of constipation can mitigate secondary issues like diverticulitis.
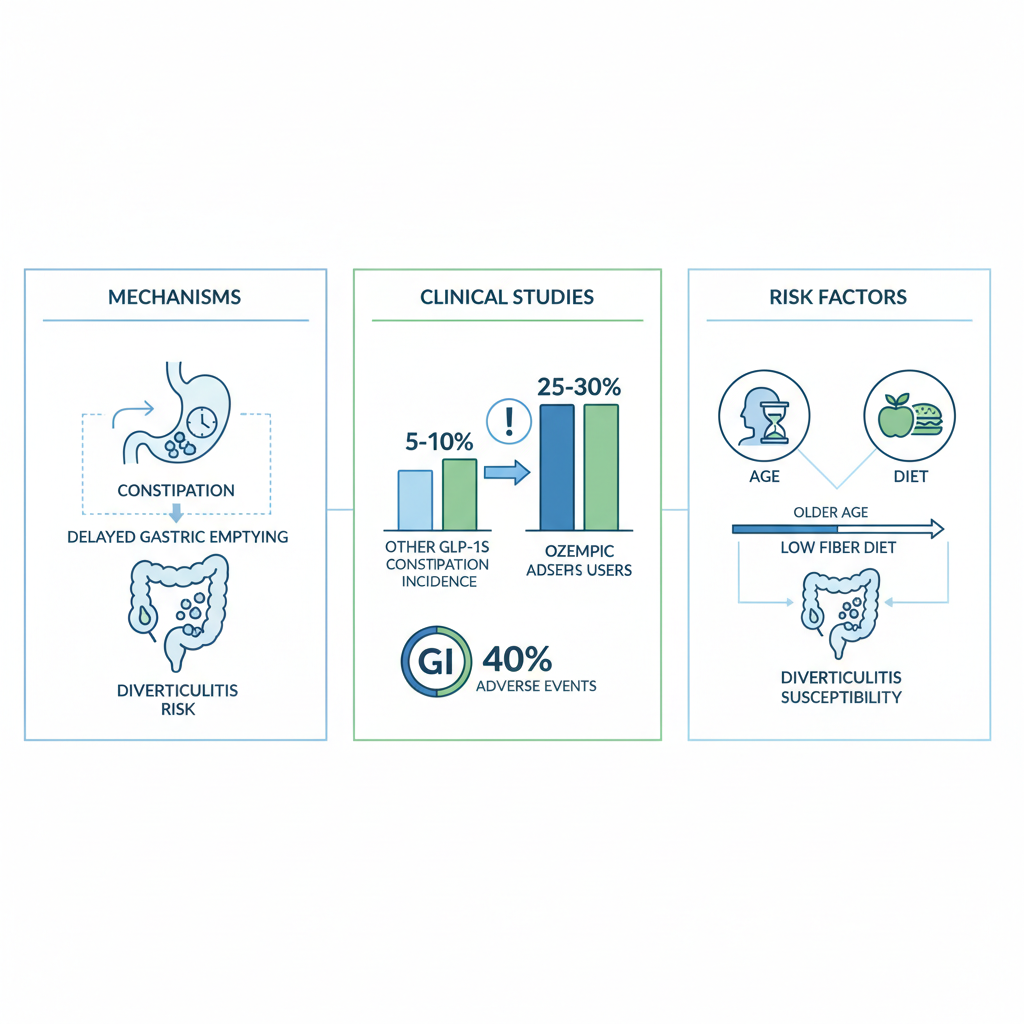
Evidence linking Ozempic to diverticulitis risks visualization
This visualization illustrates the interconnected pathways, reinforcing the need for balanced assessment.
Clinical Studies and Case Reports
Clinical evidence on the ozempic diverticulitis connection primarily emerges from observational data and post-marketing surveillance rather than large randomized trials. A PMC article on semaglutide’s GI effects reports constipation in 25-30% of users, with some cases progressing to more severe bowel complications (PMC, 2023). While direct links to diverticulitis are scarce, indirect associations appear in case reports where patients experienced acute flares amid prolonged constipation.
Trials like SUSTAIN and STEP programs noted GI adverse events in 40% of semaglutide users, including delayed motility that could indirectly foster diverticular inflammation. No study establishes causation, but patterns suggest plausible pathways: constipation-induced pressure mimicking known diverticulitis triggers. Comparative analyses with other GLP-1s show similar trends, though semaglutide’s potency amplifies risks. Caveats abound–confounding factors like diet obscure attributions–but these findings validate monitoring for symptoms. Overall, the evidence leans toward caution without alarm, prioritizing patient education.
Factors Influencing Risk
Individual variables significantly modulate the likelihood of diverticulitis flare-ups on Ozempic. Age over 60 heightens vulnerability, as colonic diverticula prevalence rises with years, amplifying pressure from motility slowdowns. Poor-fiber diets exacerbate ozempic constipation side effects, straining pouches further, while high-fiber intake may buffer risks.
Dosage plays a key role; higher weekly injections correlate with intensified gut effects. Ozempic prior authorization criteria often consider such factors for safer prescribing. Comorbidities like obesity or prior diverticulosis elevate odds, as does low hydration. Conversely, younger patients with robust diets face lower threats. Tailoring therapy–starting low and titrating slowly–mitigates these, underscoring personalized approaches.
To further delineate, consider how risk modifiers stack against protective profiles:
| Risk Modifier | High-Risk Profile | Low-Risk Profile | Impact on Flare-Ups |
|---|---|---|---|
| Age | >60 years | <50 years | Increases pressure sensitivity |
| Diet | Low-fiber intake | High-fiber, hydrated | Worsens vs. eases constipation |
| Dosage | >1mg/week | Starting/low dose | Heightens motility delay |
This breakdown, drawn from clinical insights, highlights modifiable elements. For instance, dietary adjustments can reduce semaglutide-induced bowel strain by 15-20% in some cohorts. Ultimately, awareness empowers better outcomes, blending evidence with vigilance.
Armed with this evidence, let’s explore actionable strategies for management.
Managing Ozempic with Diverticulitis
Managing Ozempic alongside diverticulitis requires careful attention to avoid exacerbating gut issues. This section provides actionable strategies to handle the ozempic diverticulitis connection, focusing on safe medication use while minimizing risks like flares and constipation. Always consult your healthcare provider for personalized advice, as this is not medical advice.
Dose Adjustments and Monitoring
When dealing with diverticulitis, timely dose adjustments can prevent complications. If you experience a flare-up, many users wonder if Ozempic can cause a diverticulitis flare up, and experts recommend pausing the medication under medical supervision to allow the gut to heal without added stress from the drug’s effects on bowel motility. According to guidance from wellness resources, holding doses during active inflammation helps reduce strain on the digestive system.
Key symptoms to monitor include abdominal pain, fever, bloating, and changes in bowel habits such as diarrhea or persistent constipation. These signs may indicate that the ozempic diverticulitis connection is triggering issues, so track them daily in a journal to share with your doctor. Regular check-ins with a gastroenterologist are essential; schedule appointments every 4-6 weeks or sooner if symptoms arise.
For precise handling, follow an ozempic usage guide that outlines when to resume dosing post-flare, typically starting at a lower dose and titrating up slowly. Consult protocols involve discussing your full medical history, including recent diverticulitis episodes, to tailor adjustments. This proactive monitoring ensures safe continuation of semaglutide while addressing handling semaglutide GI issues effectively. By staying vigilant, you can maintain benefits like weight loss without compromising gut health.
Dietary and Lifestyle Strategies
Diet plays a pivotal role in preventing bowel complications on GLP-1s like Ozempic, especially for those with diverticulitis. Aim for 25-30 grams of daily fiber from sources like fruits, vegetables, and whole grains to promote regular bowel movements and reduce constipation risks. Pair this with hydration–drink at least 8 glasses of water daily–to soften stool and support overall digestion.
Incorporate gentle exercise, such as 30 minutes of walking most days, to stimulate gut motility without straining the abdomen. These lifestyle tweaks, drawn from practical navigation tips in Ozempic treatment guides, help mitigate ozempic constipation side effects by fostering a healthier digestive environment. Avoid sudden changes; gradually increase fiber to prevent bloating.
To choose the right fiber types, consider the following comparison of soluble versus insoluble sources, which can optimize gut support while on medication:
| Fiber Type | Examples | Benefits for Ozempic Users | Considerations |
|---|---|---|---|
| Soluble | Oats, apples, beans | Absorbs water, softens stool, reduces constipation | Slower acting, may cause initial gas |
| Insoluble | Whole grains, broccoli, nuts | Adds bulk, speeds transit time, prevents flares | Increase gradually to avoid irritation |
Selecting fiber sources depends on your tolerance; soluble options suit sensitive guts during recovery, while insoluble aids long-term regularity. Personalize based on symptoms, consulting a dietitian for meal plans that align with diverticulitis needs.
Relieving Constipation Side Effects
Ozempic constipation side effects affect many users, but targeted relief can keep symptoms manageable and lower diverticulitis risks. Start with over-the-counter remedies like stool softeners (e.g., docusate) to ease passage without harsh stimulation.
Here are practical tips in numbered steps:
- Take fiber supplements such as psyllium (Metamucil) daily, mixed with plenty of water.
- Use osmotic laxatives like Miralax for quick relief, following package dosing.
- Try probiotics to restore gut balance, choosing strains like Bifidobacterium.
If symptoms persist beyond a week or include severe pain, seek medical help immediately to rule out complications. These strategies, supported by pharmacy guides, emphasize starting mild and escalating as needed.
The following table evaluates common constipation relief methods for Ozempic users, helping you weigh options to prevent diverticulitis risks:
| Method | Effectiveness | Ease of Use | Potential Side Effects |
|---|---|---|---|
| High-Fiber Diet | High for long-term | Moderate (Requires planning) | Bloating if sudden increase (Low risk) |
| Laxatives (e.g., Miralax) | Quick relief | High (Easy) | Dependency risk (Moderate) |
| Probiotics | Supportive for gut health | Variable (Daily routine) | Mild digestive upset (Low) |
When personalizing these methods, consider your baseline gut health–diet works best for mild cases, while laxatives suit acute needs. Always monitor for interactions and adjust under professional guidance to ensure safety.
For those with complex cases, advanced interventions build on these basics.
Advanced Considerations for Ozempic and Diverticulitis
For patients on Ozempic with a history of diverticulosis, advanced management requires a deeper look at potential complications. Long-term semaglutide gut effects, including the question of whether can ozempic cause diverticulitis flare up, center on chronic constipation as a key driver. Ozempic’s delayed gastric emptying can exacerbate bowel irregularity, potentially accelerating diverticula formation or progression in susceptible individuals. Studies suggest that persistent constipation increases intra-abdominal pressure, raising the risk of diverticulosis evolving into symptomatic diverticulitis over months or years. To counter this, patients should prioritize hydration and routine physical activity alongside prescribed fiber intake to maintain bowel motility and reduce strain on the colon.
When exploring alternatives, the ozempic diverticulitis connection underscores the need for tailored options if gastrointestinal side effects prove intolerable. Metformin remains a cornerstone for type 2 diabetes management, offering glycemic control with minimal impact on gut motility compared to GLP-1 agonists like Ozempic. SGLT2 inhibitors, such as empagliflozin, provide another pathway by promoting glucose excretion through the kidneys, often with diuretic effects that may indirectly support bowel regularity. These alternatives can be particularly beneficial for those with pre-existing diverticular disease, allowing continued weight management without heightening flare risks. Consulting an endocrinologist ensures seamless transitions while monitoring blood sugar stability.
Interactions add another layer of caution, especially ozempic constipation side effects combined with other drugs. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can heighten bleeding risks in diverticulitis patients by irritating the gastrointestinal lining, particularly if Ozempic slows transit time and allows prolonged exposure. Patients should discuss all over-the-counter medications with their provider, opting for acetaminophen when possible to avoid compounding mucosal stress.
The following table outlines advanced risk factors for Ozempic users versus the general population, highlighting key areas of concern.
| Factor | General Population Risk | Ozempic Users Risk | Mitigation Strategy |
|---|---|---|---|
| Constipation | 10-15% | 25-40% (Higher) | Fiber supplements (Daily) |
| Flare-Ups | 5% annually | Potentially elevated (Monitor closely) | Dose titration (Gradual) |
This comparison emphasizes personalization; for instance, higher constipation rates among Ozempic users necessitate proactive strategies to prevent escalation. Mitigation through daily fiber can stabilize bowel habits, while gradual dose adjustments minimize acute disruptions.
Monitoring forms the cornerstone of advanced GLP-1 risk management, with preventive screenings like colonoscopies recommended every 5-10 years for at-risk individuals to detect silent progression. Emerging microbiome research on GLP-1s reveals shifts in gut flora that may influence inflammation, suggesting probiotic supplementation as a supportive measure. Multidisciplinary care involving gastroenterologists and dietitians ensures comprehensive oversight. During monitoring discussions, incorporating ozempic dosing and storage tips proves essential for safe dose titration, starting low and increasing slowly to assess tolerance. Common questions arise in these advanced contexts–let’s address them next.
Frequently Asked Questions on Ozempic and Diverticulitis
Q: Can Ozempic cause diverticulitis flare up?
Ozempic does not directly cause diverticulitis flares, but semaglutide flare triggers like constipation can exacerbate existing conditions. The ozempic diverticulitis connection stems from slowed gut motility, per a PMC study on GLP-1 effects.
Q: What is the ozempic constipation side effects profile?
Ozempic constipation side effects are common due to delayed gastric emptying. Up to 20% of users report this, but it’s usually mild and manageable with lifestyle adjustments.
Q: How do you relieve constipation from Ozempic?
Increase fiber intake, stay hydrated, and exercise regularly to ease ozempic constipation side effects. Over-the-counter laxatives may help, but consult your doctor first for managing GLP-1 bowel issues.
Q: When should you hold or stop Ozempic for diverticulitis?
Hold the dose if severe symptoms arise and contact your healthcare provider. Long-term risks are low, but professional guidance ensures safety, as noted in PMC research on GI impacts.
Q: How to manage diverticulitis while on Ozempic?
Monitor symptoms closely and follow a high-fiber diet. Discuss dose adjustments with your doctor to balance benefits and the ozempic diverticulitis connection. Always seek medical advice for personalized care.
Key Takeaways on Ozempic and Diverticulitis Management
Ozempic offers semaglutide safety insights for weight management, but understanding the ozempic diverticulitis connection remains key. While no direct causation exists, ozempic constipation side effects could indirectly contribute to a can ozempic cause diverticulitis flare up.
- Proactive Strategies: Prioritize fiber-rich diets and hydration to mitigate gastrointestinal issues, alongside regular monitoring for holistic gut care on GLP-1s.
- Risk-Benefit Balance: For many, Ozempic’s benefits in weight loss and metabolic health outweigh potential concerns, including ozempic common long term risks like ongoing GI discomfort.
- Empowerment Tip: Always consult healthcare providers for tailored plans, navigating your wellness journey holistically as emphasized in expert guidance.

