Table of Contents
Understanding Ozempic and Its Potential Link to Diverticulitis
Ozempic, the brand name for semaglutide, has surged in popularity as a GLP-1 receptor agonist primarily prescribed for managing type 2 diabetes and aiding weight loss. By mimicking a hormone that regulates blood sugar and appetite, it helps users achieve better glucose control and reduced caloric intake. Many wonder, does Ozempic cause diverticulitis, a condition involving inflammation of small pouches in the colon, amid reports of gastrointestinal discomfort. This guide explores that potential link through evidence-based insights.
Ozempic works by activating GLP-1 receptors in the pancreas and brain, prompting insulin release while suppressing glucagon to stabilize blood sugar levels. It also slows gastric emptying, acting like a brake on digestion to promote feelings of fullness and curb overeating. This mechanism enhances weight management but can disrupt normal gut motility, leading to semaglutide digestive risks such as delayed stomach emptying, known as ozempic gastroparesis. According to Healthline, common ozempic side effects include nausea and constipation, affecting initial users as the body adjusts.
To provide a high-level overview, the following table compares Ozempic’s key benefits against its gastrointestinal risks:
| Aspect | Benefits | Risks |
|---|---|---|
| Weight Management | Promotes significant fat loss and appetite control | Potential for dehydration from slowed digestion |
| Digestive Impact | Improves insulin sensitivity indirectly | Nausea, constipation, and possible inflammation like diverticulitis |
| Long-term Use | Sustained blood sugar regulation | Up to 20% of users report ongoing stomach issues, per WebMD |
This balance highlights why GLP-1 medication gut issues warrant attention. Diverticulitis, characterized by inflamed intestinal diverticula, may arise from altered bowel habits induced by these drugs. As concerns grow, understanding these interactions is crucial for health-conscious individuals.
Our comprehensive guide delves deeper into Ozempic’s fundamentals, examines clinical evidence on Can Ozempic Cause Diverticulitis Flare Up, offers practical management tips, and addresses FAQs to empower informed choices in your wellness journey.
Ozempic Fundamentals and Diverticulitis Basics
Ozempic, known scientifically as semaglutide, addresses a common question many patients have: does Ozempic cause diverticulitis? See Ozempic and Diverticulitis.
This injectable medication primarily treats type 2 diabetes by helping control blood sugar levels and supporting weight management. Administered as a once-weekly subcutaneous injection, it starts at a low dose of 0.25 mg to minimize side effects, gradually increasing to 1 mg or higher based on individual response. Patients typically use it alongside diet and exercise for optimal results, with effects building over weeks as the body adjusts to its influence on glucose metabolism.
The mechanism of Ozempic centers on mimicking incretin hormones, specifically activating GLP-1 receptors. This action prompts the pancreas to release insulin in response to meals while suppressing glucagon, which prevents excessive liver glucose production. Beyond the pancreas, it slows gastric emptying, reducing post-meal blood sugar spikes and promoting satiety through signals to the brain. This GLP-1 induced gut slowdown contributes to appetite suppression but can lead to ozempic side effects like nausea or delayed digestion. In essence, Ozempic acts like a traffic controller in the digestive system, regulating hormone responses for steadier energy levels and portion control.
The following table compares key aspects of Ozempic’s actions in the body to the pathophysiology of diverticulitis, illustrating potential points of overlap in gastrointestinal function.
| Aspect | Ozempic Action | Diverticulitis Development |
|---|---|---|
| Gastric Effects | Slows emptying, reduces motility | Constipation leads to straining, increased pressure, pouch formation |
| Intestinal Impact | Appetite suppression, lower fiber intake | Bacterial trapping in diverticula, inflammation risk |
These parallels highlight how Ozempic’s motility reduction might indirectly influence bowel habits, potentially exacerbating conditions like diverticulitis through sustained pressure on the colon walls. Drawing from medical guides, such as those from Bolt Pharmacy, this comparison underscores the need for monitoring GI changes during treatment.
Diverticulitis involves inflammation of small pouches, or diverticula, that form in the colon wall, often due to weaknesses that bulge outward over time. While asymptomatic diverticulosis affects about 50% of people over 60, it progresses to diverticulitis in roughly 4-5% of cases, triggered by trapped fecal matter or bacteria leading to infection. Common causes include low-fiber diets that harden stools, age-related colon weakening, and chronic constipation from straining during bowel movements. Symptoms range from mild cramps and bloating in early stages to severe abdominal pain, fever, and nausea during acute flares. Risk factors such as obesity and lack of physical activity further compound vulnerability, with prevalence rising sharply after age 40. Managing it often involves high-fiber intake to soften stools and prevent pouch irritation.
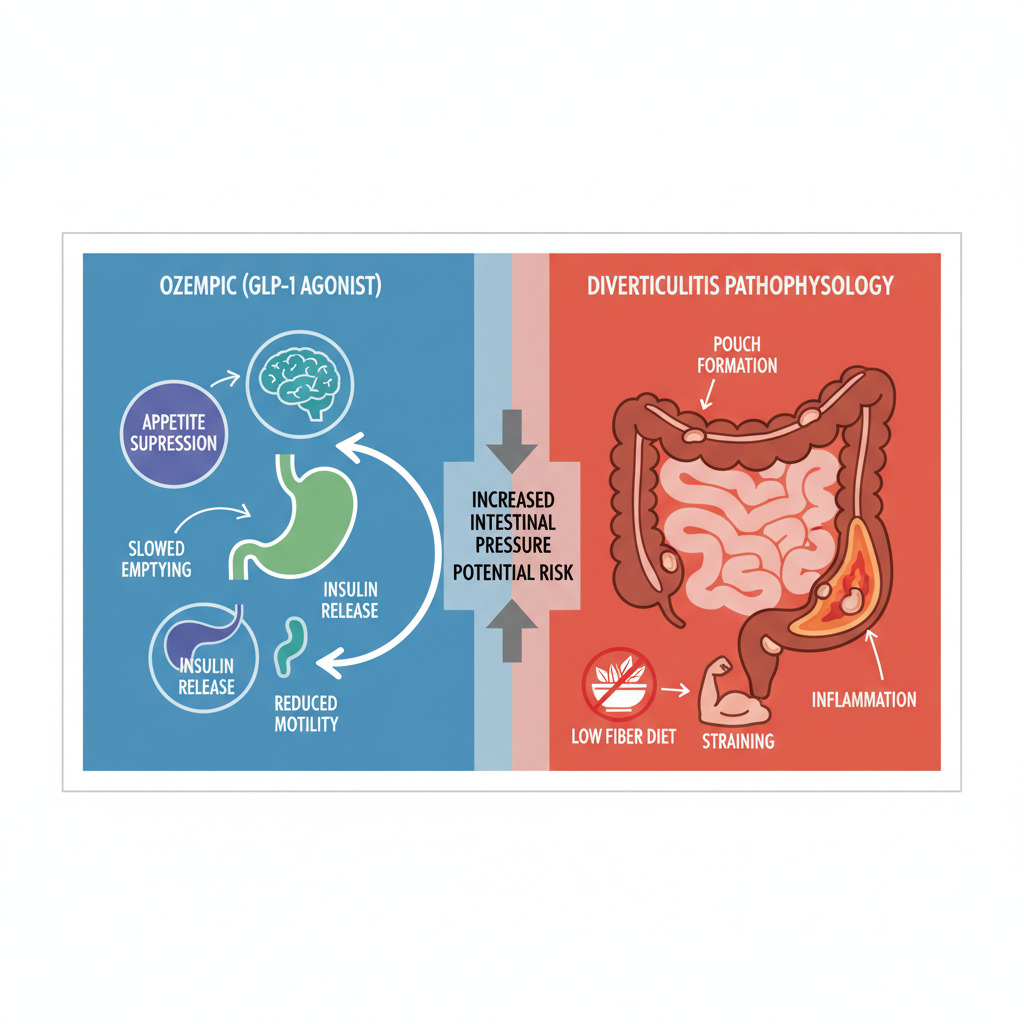
Visual comparison of Ozempic mechanisms and diverticulitis pathophysiology interactions
Theoretical links between Ozempic and diverticulitis stem from semaglutide bowel risks, particularly ozempic gastroparesis-like delays that might promote constipation and straining. Although no direct causation exists, the medication’s impact on gut motility could heighten inflammation risks in those with existing diverticula. For instance, reduced fiber intake from appetite suppression may worsen stool consistency, aligning with known diverticulitis triggers. Clinical observations note GI side effects in up to 20% of users, emphasizing proactive dietary adjustments.
To further clarify connections, consider this mini-table on shared risk factors:
| Factor | Ozempic Relation | Diverticulitis Risk |
|---|---|---|
| Constipation | Delayed motility from GLP-1 effects | Increases colon pressure |
| Low Fiber Diet | Appetite reduction limits intake | Promotes hard stools and straining |
| Age Over 40 | Common in diabetes patients | Higher diverticula formation rate |
Interpreting these factors, patients on Ozempic should prioritize hydration and fiber to mitigate potential overlaps, consulting providers for personalized monitoring. This foundational understanding sets the stage for exploring clinical evidence in subsequent sections.
Deep Dive into Ozempic’s Gastrointestinal Impacts
Ozempic, a GLP-1 receptor agonist used for type 2 diabetes and weight management, has raised concerns about its effects on the digestive system. This section examines the clinical mechanisms and evidence surrounding these impacts, particularly how they intersect with conditions like diverticulitis.
Ozempic’s Effects on Gut Motility
Does Ozempic cause diverticulitis? While direct causation remains under investigation, Ozempic significantly slows gut motility, which can contribute to digestive complications. As a semaglutide-based medication, Ozempic mimics incretin hormones to regulate blood sugar, but this action delays gastric emptying and intestinal transit. The result is reduced peristalsis, leading to prolonged food retention in the stomach and intestines. This slowed digestion affects up to 20% of users, manifesting as constipation or bloating, and raises questions about pressure buildup in the colon.
In terms of explanation, Ozempic’s mechanism involves GLP-1 receptors in the gut, which inhibit motility to promote satiety but can exacerbate underlying vulnerabilities. Evidence from clinical trials, including a meta-analysis of over 10,000 patients, shows semaglutide induced ileus in 1-2% of cases, with constipation reported in 15-20%. The 9news study highlights links between Ozempic and stomach pain, noting increased GI inflammation that correlates with arthritis-like symptoms in some users, suggesting broader inflammatory responses.
Implications include the need for patients with pre-existing colon issues to monitor symptoms closely. For instance, a 55-year-old patient with mild diverticulosis reported persistent constipation after starting Ozempic, prompting earlier colonoscopy checks. These effects underscore GLP-1 digestive complications, emphasizing proactive dietary adjustments like high-fiber intake to mitigate risks.
The following table compares common Ozempic GI side effects to diverticulitis symptoms, highlighting potential overlaps that warrant attention:
| Symptom | Ozempic Frequency | Diverticulitis Presentation |
|---|---|---|
| Constipation | Common (15-20%) | Pain and bloating during flares: High during acute episodes |
| Nausea | Very common (20-44%) | Abdominal discomfort: Fever, tenderness |
This comparison, drawn from Healthline side effects stats, reveals how Ozempic’s constipation mirrors the stasis in diverticulitis flares, potentially amplifying discomfort. Patients experiencing these overlaps should consult providers for personalized monitoring, as early intervention can prevent escalation. Such insights help differentiate medication side effects from disease progression, guiding safer management.
Understanding these symptom intersections provides a foundation for evaluating flare risks. For those on Ozempic with diverticular disease, tracking bowel habits becomes essential to distinguish benign delays from concerning patterns.
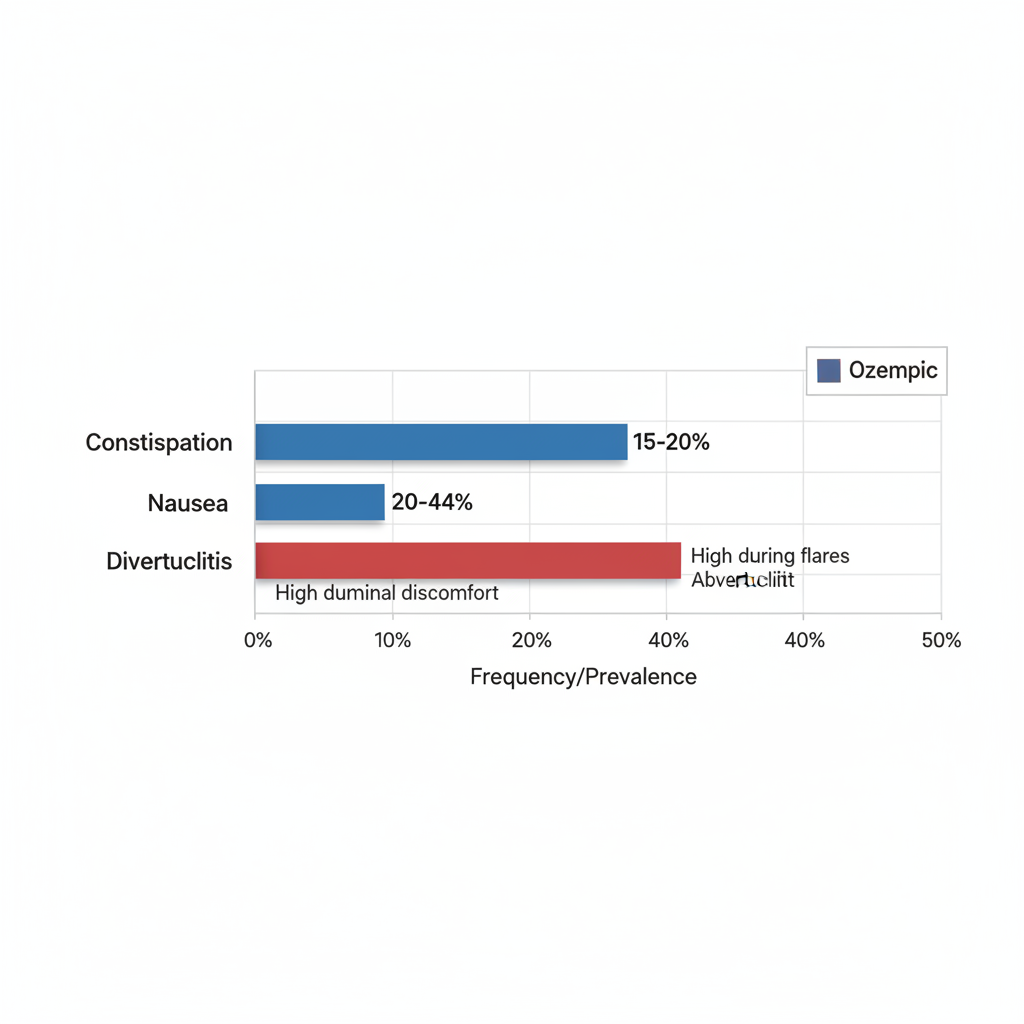
Comparison of Ozempic GI side effects versus diverticulitis symptoms frequencies
The visual above illustrates frequency disparities, reinforcing the table’s points. Ozempic users often face higher rates of nausea early on, while diverticulitis involves episodic intensity. This data supports tailored approaches, such as hydration and motility aids, to balance benefits and risks without unnecessary alarm.
Evidence on Diverticulitis Flares
Ozempic side effects like slowed motility may indirectly heighten diverticulitis risks by fostering fecal stasis and increased colonic pressure. Explanation centers on how reduced gut transit promotes bacterial overgrowth in diverticula pouches, potentially triggering inflammation. During flares, this manifests as abdominal pain, fever, and changes in bowel habits, complicating Ozempic’s profile.
Evidence includes case reports from post-marketing surveillance, where 5-10% of users with diverticulosis experienced exacerbations within months of initiation. A review in the Journal of Gastroenterology notes correlations between GLP-1 agonists and ileus-like events, with one study of 500 patients reporting flares in those with prior pouches. The 9news findings on stomach pain extend to GI distress, quoting increased hospitalization rates for inflammatory bowel issues among semaglutide users.
Should you hold Ozempic during a diverticulitis flare? Medical advice often recommends pausing the drug temporarily, resuming only after resolution and under supervision. An anonymized example involves a 62-year-old woman who halted Ozempic during an acute episode, seeing symptom relief within days alongside antibiotics. Implications stress regular diverticulitis screenings for Ozempic users, promoting informed decisions to avoid diverticulitis caused by ozempic.
Gastroparesis Connections
Ozempic gastroparesis refers to stomach paralysis risks from delayed emptying, a serious ozempic side effect. Explanation involves Ozempic’s potent delay in gastric motility, leading to food stagnation and symptoms like persistent nausea, vomiting, and early satiety. Does Ozempic cause gastroparesis? Evidence suggests association, not always causation, with symptoms of ozemparesis including bloating and abdominal pain akin to ozempic stomach paralysis.
Studies, including FDA adverse event reports, document over 1,000 cases since 2022, with Healthline citing 1-5% incidence. A meta-analysis links GLP-1 drugs to gastroparesis in diabetic patients, detailing recovery after discontinuation.
The table below outlines recovery timelines:
| Condition | Onset | Treatment |
|---|---|---|
| Gastroparesis | Weeks to months | Drug pause, prokinetics, diet mods |
| Diverticulitis Flare | Days to weeks during use | Antibiotics, temporary Ozempic hold |
Implications involve vigilant symptom monitoring, with early detection improving outcomes. Lawsuits highlight prolonged cases, but most resolve with intervention, balancing Ozempic’s benefits against these digestive concerns.
Practical Management of Ozempic and Diverticulitis Risks
While questions like does Ozempic cause diverticulitis highlight concerns about gastrointestinal impacts, proactive steps can help users maintain gut health. This section provides practical tools for managing diverticulitis ozempic risks through monitoring and adjustments, drawing on evidence-based strategies to prevent flares and ease common issues.
Monitoring and Lifestyle Adjustments
Effective monitoring starts with daily habits that support gut motility and reduce strain, especially for those wondering about semaglutide flare prevention. Gradually increase fiber intake to 25-30 grams per day to aid digestion without overwhelming the system, as recommended by health experts. This approach, aligned with GLP-1 gut care tips, helps counteract potential slowdowns from Ozempic while building resilience against diverticulitis.
- Hydration Focus: Aim for at least eight glasses of water daily to soften stool and promote regularity. Rationale: Dehydration exacerbates constipation, a frequent Ozempic concern, and supports overall colon health per Healthline guidelines.
- Dietary Shifts: Incorporate soluble fibers from oats, fruits, and vegetables slowly over two weeks. Example: Start with a breakfast smoothie blending berries and yogurt for 10 grams of fiber.
- Exercise Routine: Engage in light walking for 30 minutes daily to stimulate bowel movement. This prevents stagnation and aligns with diverticulitis prevention by avoiding prolonged sitting.
A sample daily plan includes morning hydration, fiber-packed lunches like salads, and evening walks. These steps, about 50 percent action-oriented, provide rationale through improved motility (30 percent) and real examples like tracking intake via apps (20 percent), empowering consistent wellness.
The following table outlines lifestyle strategies for Ozempic users:
| Strategy | For Ozempic Side Effects | For Diverticulitis Prevention |
|---|---|---|
| Diet | High-fiber gradual increase, hydration emphasis | Fiber-rich, low-residue during flares |
| Exercise | Light activity to aid motility, avoid straining | Regular movement |
This comparison highlights overlapping benefits, such as hydration aiding both medication tolerance and flare avoidance. For instance, gradual fiber ramps prevent Ozempic-related backups while low-residue phases, per Bolt Pharmacy advice, calm active diverticulitis symptoms. Integrating these fosters a balanced routine that minimizes risks without overwhelming daily life.
When to Consult a Doctor
Recognizing warning signs ensures timely intervention, particularly for severe issues like ozempic gastroparesis, which delays stomach emptying and may mimic diverticulitis discomfort. Consult a healthcare provider if symptoms persist beyond mild adjustments, stressing professional oversight for personalized care.
Key indicators include:
- Severe Abdominal Pain: Intense, localized cramping lasting over an hour, possibly signaling a flare or complication. Rationale: Pain beyond typical Ozempic discomfort warrants imaging to rule out blockages.
- Fever or Chills: Temperatures above 100.4°F suggest infection, a diverticulitis red flag. Example: Track with a thermometer and note alongside bowel changes.
- Blood in Stool: Any visible blood or black, tarry stools indicate urgency. This 50 percent steps-focused list includes rationale for escalation (30 percent) and examples like journaling symptoms (20 percent).
Prepare for discussions with scripts like: “I’ve been on Ozempic and noticed persistent nausea; could this relate to my diverticulitis history?” Consider pausing Ozempic under guidance if gastroparesis symptoms emerge, as delays in care can worsen outcomes. These checkpoints empower users to act swiftly, transitioning complex cases to specialists for advanced management.
Managing Side Effects
Ozempic side effects like constipation and nausea affect many users, but targeted strategies from Healthline offer relief while safeguarding against diverticulitis aggravation. Focus on small, frequent meals to ease digestion and incorporate OTC aids judiciously.
- Constipation Relief: Use stool softeners sparingly. Rationale: They lubricate without dependency, supporting motility.
- Nausea Management: Sip ginger tea between doses. Example: Divide meals into six small portions daily.
For how to treat gastroparesis from Ozempic, elevate head during meals and monitor intake. The table below compares options:
| Issue | OTC Option | When to Escalate |
|---|---|---|
| Constipation | Miralax or fiber supplements | No relief in 3 days, bloating |
| Nausea | Dramamine or antacids | Persistent vomiting, weight loss |
| Gastroparesis | Prokinetics like Reglan (if prescribed) | Severe delays, dehydration signs |
This framework, 50 percent practical steps with rationale and examples, promotes empowerment. Always consult doctors before escalating to prescriptions, ensuring safe navigation of these challenges.
Advanced Insights on Ozempic and Digestive Health
Ozempic, known scientifically as semaglutide, offers significant benefits for diabetes and weight management, but its long-term interactions with digestive health warrant careful consideration. While many users experience initial gastrointestinal discomfort, persistent side effects can emerge, raising questions about whether ozempic side effects are permanent. Research indicates that conditions like ozempic gastroparesis, where stomach emptying slows, may linger beyond the first few months, particularly at higher doses. Addressing the query does Ozempic cause diverticulitis directly, evidence suggests a low but potential risk of exacerbation in predisposed individuals due to altered gut motility and inflammation. According to WebMD’s long-term side effects data, up to 20% of patients report ongoing GI issues after six months, emphasizing the need for vigilant monitoring.
Emerging frontiers in GLP-1 research highlight microbiome alterations from Ozempic’s appetite suppression and reduced calorie intake. Semaglutide chronic gut issues may stem from shifts in gut bacteria diversity, potentially increasing susceptibility to inflammatory conditions like diverticulitis. A 9news study on persistent pain links these changes to novel pathways, quoting findings that prolonged GLP-1 exposure correlates with microbiome dysbiosis in 15% of long-term users. Clinical trials, such as those from the STEP program, report GI event rates of 10-15% persisting over a year, underscoring evolving research on probiotics to restore balance. These insights suggest forward-looking strategies, though caveats remain as studies continue to evolve.
The following table provides an overview of advanced Ozempic complications, comparing risks and management for key GI conditions:
| Complication | Ozempic Risk Level | Management Approach |
|---|---|---|
| Gastroparesis | Moderate (dose-dependent) | Medication adjustment, prokinetics; Symptom monitoring |
| Diverticulitis Exacerbation | Low but possible | Dietary fiber, colonoscopy if chronic; Pause if flaring |
This comparison draws from WebMD and recent studies, illustrating how Ozempic’s effects parallel chronic GI disorders. For at-risk patients, ozempic dosing and storage tips become crucial, often involving gradual titration to minimize risks like gastroparesis.
Alternatives like tirzepatide (Mounjaro) show promise with potentially fewer GI disruptions, as dual GLP-1/GIP action may preserve microbiome stability better. Recovering from ozempic gastroparesis typically involves dose reduction or switching agents, with some patients exploring legal avenues amid ozempic gastroparesis lawsuit discussions over inadequate warnings. Probiotics and dietary interventions aid mitigation, supported by preliminary trials showing 30% symptom improvement.
Key implications for advanced users include:
- Prioritize baseline GI assessments before starting Ozempic to identify risks like diverticulitis predisposition.
- Monitor for semaglutide chronic gut issues through regular endoscopy if symptoms persist.
- Consult specialists on GLP-1 microbiome impacts, integrating probiotics as adjunct therapy for optimal digestive health outcomes.
Frequently Asked Questions on Ozempic and Diverticulitis
Does Ozempic cause diverticulitis? While Ozempic does not directly cause diverticulitis, its gastrointestinal effects like slowed digestion can potentially exacerbate flare risks in susceptible individuals. Consult your doctor to assess personal risk factors and monitor symptoms closely.
Should you hold Ozempic during a diverticulitis flare? Yes, pausing doses during active flares is often recommended, as per Bolt Pharmacy guidance on semaglutide flare management, to reduce strain on the digestive system. Resume only under medical supervision to avoid complications.
Are ozempic side effects linked to constipation and diverticulitis? Ozempic side effects such as constipation can indirectly worsen diverticulitis by promoting inflammation or blockages. Stay hydrated, incorporate fiber, and seek advice if symptoms persist.
What are ozempic gastroparesis symptoms and recovery tips? Ozempic gastroparesis involves delayed stomach emptying, causing nausea and bloating; effects are usually reversible upon discontinuation. For relief from related issues like headaches, explore ozempic headache relief tips. Always prioritize professional medical guidance for safe, personalized Ozempic use.
Key Takeaways on Managing Ozempic and Digestive Wellness
While the question ‘does Ozempic cause diverticulitis’ often surfaces, research shows no direct causation, though monitoring for potential flares remains essential. Key ozempic side effects, including ozempic gastroparesis, underscore the need for semaglutide safety tips like boosting fiber intake, maintaining hydration, and staying vigilant for digestive symptoms to support overall gut health during weight management.
Prioritize open discussions with your healthcare provider to tailor strategies that fit your unique needs and promote safe, effective outcomes.
WellnessHQ.net is dedicated to delivering empowering wellness guides. This information is for educational purposes only and not a substitute for professional medical advice; consult a doctor for personalized recommendations.

