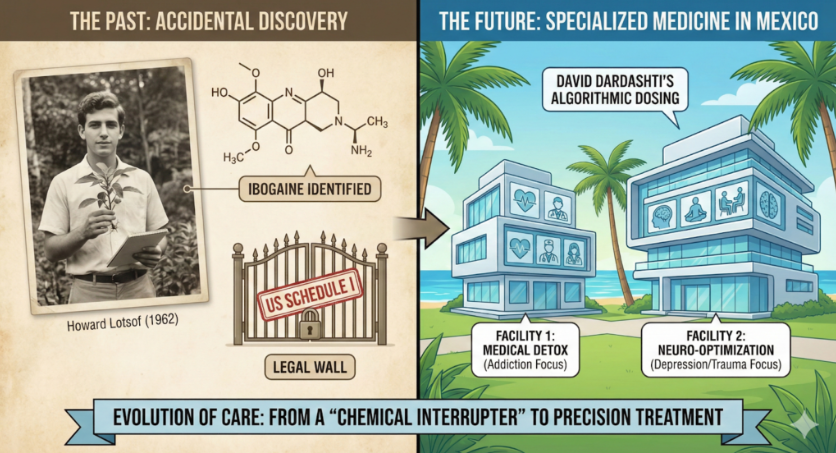
In the history of medicine, the most profound discoveries are often accidents. Penicillin was a moldy petri dish; the X-ray was a glowing screen in a dark lab. And the cure for the modern opioid crisis? It was discovered in 1962 by a 19-year-old heroin addict named Howard Lotsof, who was simply looking for a new high.
Lotsof, a young man from New York, was experimenting with a West African shrub called Tabernanthe iboga. He expected a hallucinogenic trip. What he got was a miracle. After a 30-hour journey, he woke up to a realization that defied the known laws of addiction medicine: he had no cravings. He had no withdrawal symptoms. He was, for the first time in years, completely free.
Howard Lotsof spent the rest of his life fighting to bring this discovery—Ibogaine—to the world. He viewed it not just as a drug, but as a “chemical interrupter” that could break the chains of dependency in a single session. However, the path from that discovery to safe, accessible treatment has been a long, legal, and logistical odyssey that has ultimately led to the shores of Mexico.
Here is the story of that journey, the legal hurdles that shaped it, and how modern American ingenuity has transformed a tribal sacrament into a state-of-the-art medical protocol.
The Legal Wall: Why the Cure is Exiled
Despite Lotsof’s tireless advocacy and a flurry of patents in the 1980s, the United States government classified Ibogaine as a Schedule I substance. This classification, shared by drugs like heroin and LSD, defined Ibogaine as having “no currently accepted medical use and a high potential for abuse.”
This ruling created a tragic paradox. The very substance that could solve the opioid epidemic was banned by the same government fighting that epidemic. Because Schedule I status makes clinical trials nearly impossible to fund or approve, research in the U.S. ground to a halt.
But addiction did not stop. It exploded.
As the opioid crisis morphed from heroin to OxyContin to Fentanyl, the desperate need for a solution pushed patients to look beyond American borders. They looked to jurisdictions where medical freedom still existed. They looked to Mexico.
The Rise of American Standards in Mexico
In the early days, “going to Mexico for Ibogaine” often meant visiting unregulated, makeshift clinics with little safety oversight. But in the last decade, a shift has occurred. American businessmen and medical professionals, recognizing the potential of this medicine, have migrated south to build facilities that rival the safety standards of any U.S. hospital.
This new wave of Ibogaine treatment centers—centered largely in Baja and the Riviera Maya—operates under a hybrid model:
- Legal Jurisdiction: They operate under Mexican law, where Ibogaine is unregulated and legal to administer.
- American Safety Protocols: They import U.S. standards of care. This includes mandatory ACLS (Advanced Cardiac Life Support) certification for all staff, the use of board-certified cardiologists, and the implementation of continuous cardiac telemetry during treatment.
These facilities have effectively created a “medical safety bubble.” They utilize rigorous intake screenings to rule out contraindications (such as pre-existing heart conditions) and employ modern medical equipment to monitor the QTc interval—a critical safety metric that Lotsof himself could only have dreamed of monitoring in the 1960s.
The Psychology of the Journey
For many patients, the fact that Ibogaine treatment requires travel is not a bug; it is a feature.
Addiction is often tied to environment. The addict’s home city is a minefield of triggers—the corner where they bought drugs, the room where they used, the friends who enabled them. Healing requires a break from this geography.
The journey to Mexico functions as a modern-day pilgrimage. It is a psychological severance from the “old life.” By physically leaving the environment of their trauma and traveling to a place of natural beauty—often featuring beaches, jungles, and sunlight—patients begin the neuroplastic change before they even take the medicine. They are signaling to their subconscious that they are leaving the scene of the crime and entering a sanctuary of healing.
The Next Evolution: Specialized Care by David Dardashti
As the industry matures, it is moving from “general” treatment to “specialized” medicine. Leading this charge is Ibogaine by David Dardashti, a facility that has pioneered the use of algorithmic dosing.
For years, Ibogaine clinics treated everyone together: the heroin addict detoxing from fentanyl sat next to the veteran processing PTSD, who sat next to the executive treating burnout. While they all shared a desire for healing, their medical and psychological needs were vastly different.
- The Addict needs medical stabilization, constant vital monitoring, and a quiet, low-stimulus environment to manage detox.
- The Depression/Trauma Patient is not detoxing. They are physically stable but psychologically fragile. They need distinct amenities—integration therapy, somatic bodywork, and a different “set and setting” to process their grief or trauma.
Recognizing this, Ibogaine by David Dardashti has recently expanded operations by opening a second facility.
This expansion is a major leap forward for the industry. The intent is to physically and energetically separate these two cohorts.
- The Detox Facility: Focused entirely on the medical interruption of addiction. It is equipped for high-level monitoring and physical stabilization.
- The Neuro-Optimization Facility: Focused on non-addiction issues like depression, anxiety, and PTSD. This environment is curated for deep introspection, featuring amenities that support psychological expansion rather than physical detox.
This specialization allows the medical team to tailor the Ibogaine algorithm even further. A trauma patient does not need the same “flood dose” as a fentanyl addict; they often benefit from “psycholytic” dosing that allows for greater recall and integration. By separating the facilities, David Dardashti is ensuring that each patient receives a protocol perfectly tuned to their specific pathology.
Conclusion: Howard Lotsof’s Legacy Lives On
Howard Lotsof passed away in 2010, but his vision has not only survived; it has evolved. What started as an accidental discovery in a New York apartment has grown into a sophisticated, multi-facility medical discipline in Mexico.
Today, thanks to the bridge built by American innovators and Mexican medical freedom, the “cure” is no longer a myth. It is a safe, accessible, and increasingly specialized reality for those willing to make the journey.
For more information visit https://ibogaineclinic.com/ibogaine-centers-in-mexico/